Intraoperative MMF With Minne Ties Agile MMF During Open Reduction Internal Fixation of a Bilateral Mandible Fracture
A 22-year-old African American female presented to the University of Louisville Hospital Emergency Department after being assaulted and sustaining facial injuries. The Emergency Department evaluated the patient, and they obtained a CT head, cervical spine, and facial bones. She sustained isolated bilateral mandible fractures but no other injuries. Other past medical history included depression, anxiety, and substance abuse.
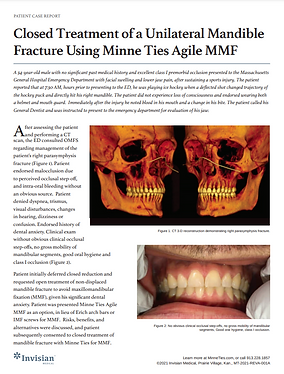
The patient was in no acute distress and was awake, alert, and oriented. Her nose was midline, her gross visual acuity was intact, and her maxilla was stable. Her mandible was grossly mobile. There was clearly a displaced open right parasymphysis fracture which extended between teeth numbers 26 & 28. There was also an open left angle fracture that was appreciated. Tooth numbers 26 & 28 were stable within the alveolus, while tooth number 27 was avulsed. Tooth number 17 was partially impacted and mobile. The patient had fair dentition.
The patient was presented with treatment options, including closed management and open reduction. The patient did not want to have maxillomandibular fixation for six weeks and opted to proceed with open reduction and internal fixation. Minne Ties were a viable option for intra-operative MMF due to the patient’s good dentition, and were chosen over other MMF methods based on less time to apply and remove, reduced trauma to the dentition and ease of application.

The patient was intubated in the OR via standard nasotracheal intubation and prepped and draped in a typical fashion. Site number 27 was debrided, and several loose bone fragments were identified and removed. Tooth #17 was mobile and extracted.
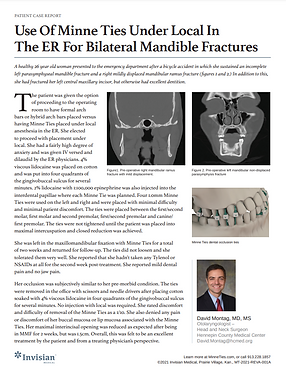
Three large (18g) Minne Ties were placed on the right side, posterior to anterior, two large were placed on the left side, and one large was placed between her central incisors. Each device was left loose until all were applied. The patient came into occlusion well, and it was noted that occlusion was stable. Total application of the devices took approximately 5 minutes.
The right-sided parasymphysis fracture was first exposed, and the mental nerve was dissected and skeletonized. Following this, the left angle fracture was exposed. Adequate exposure of the fractures was obtained, both proximal and distal. Both fractures were well-reduced, and the patient remained in excellent occlusion.
The right parasymphysis fracture was first fixated by placing a 2.5 mm locking reconstruction plate on the inferior border. With satisfactory anatomic reduction and occlusion, a 1.5 mm lateral border plate was placed on the left angle fracture. The patient’s occlusion was solid throughout this process. The patient was in maxillomandibular fixation with Minne Ties during the entire procedure.


The Minne Ties were then removed, which took less than one minute, and the patient came into occlusion nicely and passively. Her surgical sites were irrigated, and the angle incision was closed, followed by closure of the right-sided incision. The oral cavity was irrigated, the throat pack was pulled, and the patient was extubated.
The patient demonstrated pre-morbid occlusion and adequate healing during her 2-week follow-up visit. The patient’s good dentition and history of anxiety made her an ideal candidate for Minne Ties, which saved time compared to the alternative MMF methods that were considered.
With a total application time of five minutes and removal time of one minute, Minne Ties significantly reduced total operative time, were minimally traumatic to the patient’s dentition and gingiva, reduced the risk of wire stick injuries for the providers and surgical staff, and produced strong and stable MMF and occlusion throughout the case, resulting in an excellent surgical outcome.


.jpg)